Request for Qualifications
Burnaby Patient Medical Home for Priority Populations
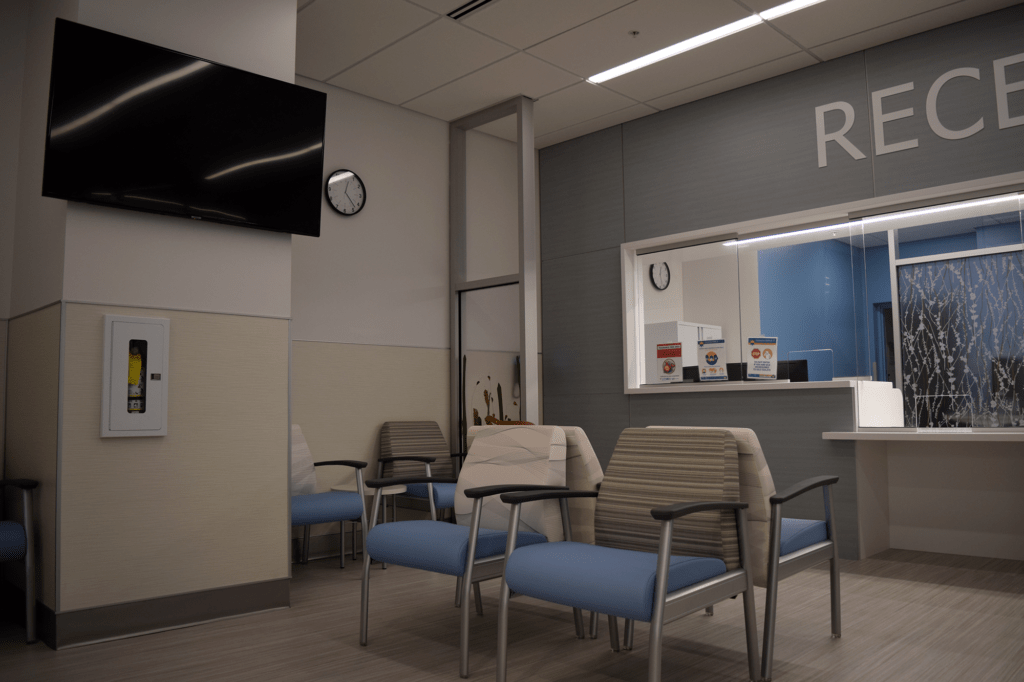
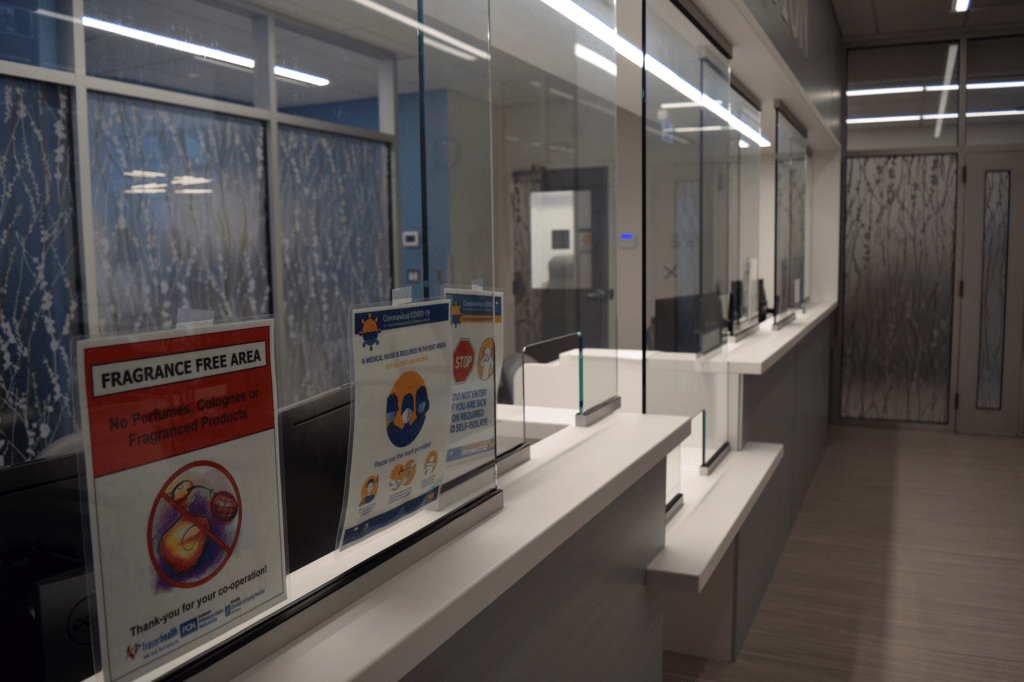
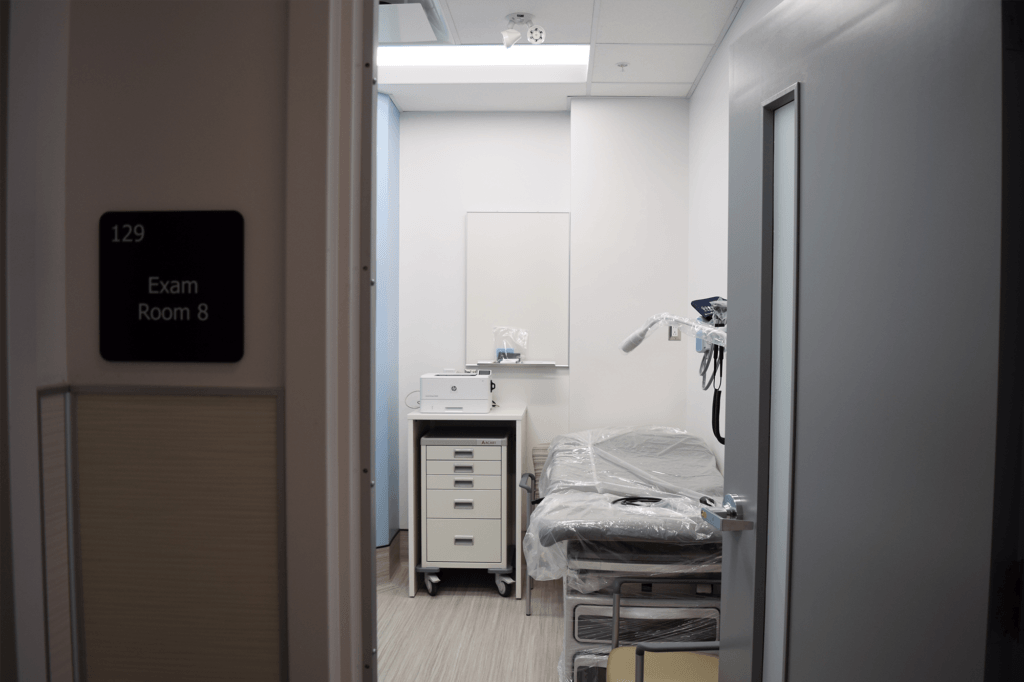
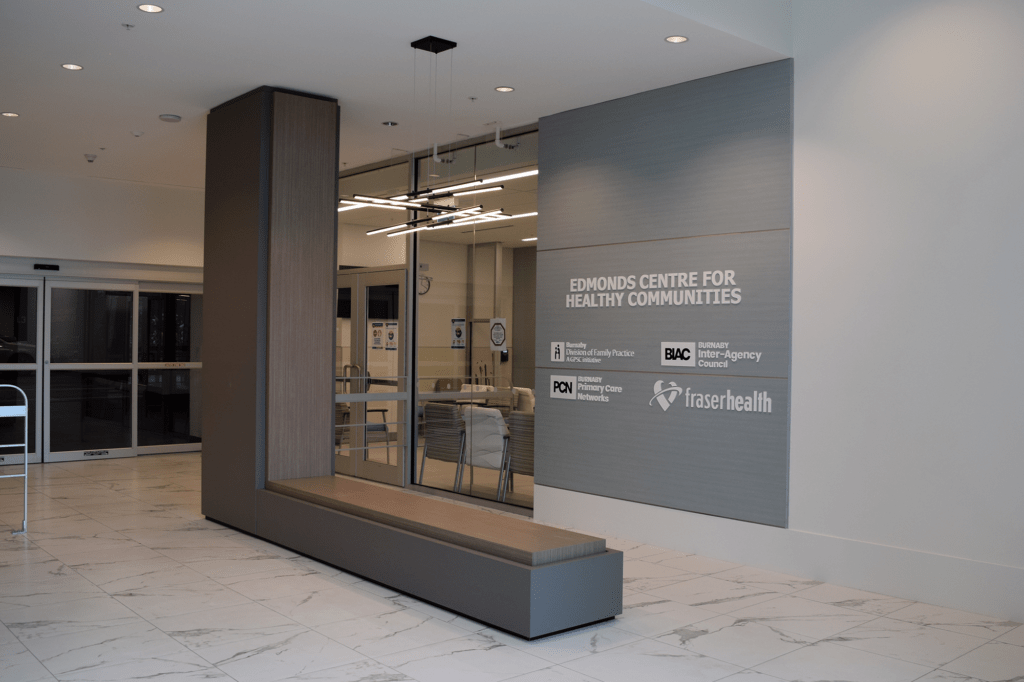
A part of the Edmonds Centre for Healthy Communities
This RFQ is now closed. Thank you to all who responded!
The Burnaby Primary Care Networks is releasing this Request for Qualifications (RFQ) to identify a not-for-profit organization (or organizations) to operate a new clinic focused on primary care and health promotion for priority populations.
*Please note there has been an update to the Response Template, section “3.5 Review and Selection”, since the application opening. (Updated Oct 18, 5pm)
OVERVIEW
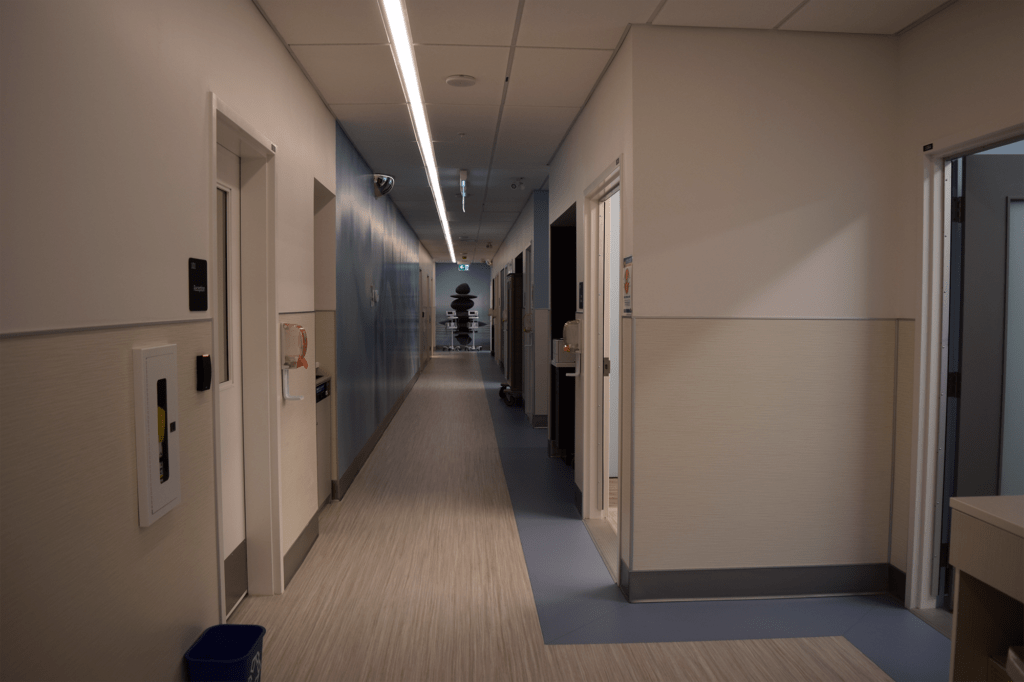
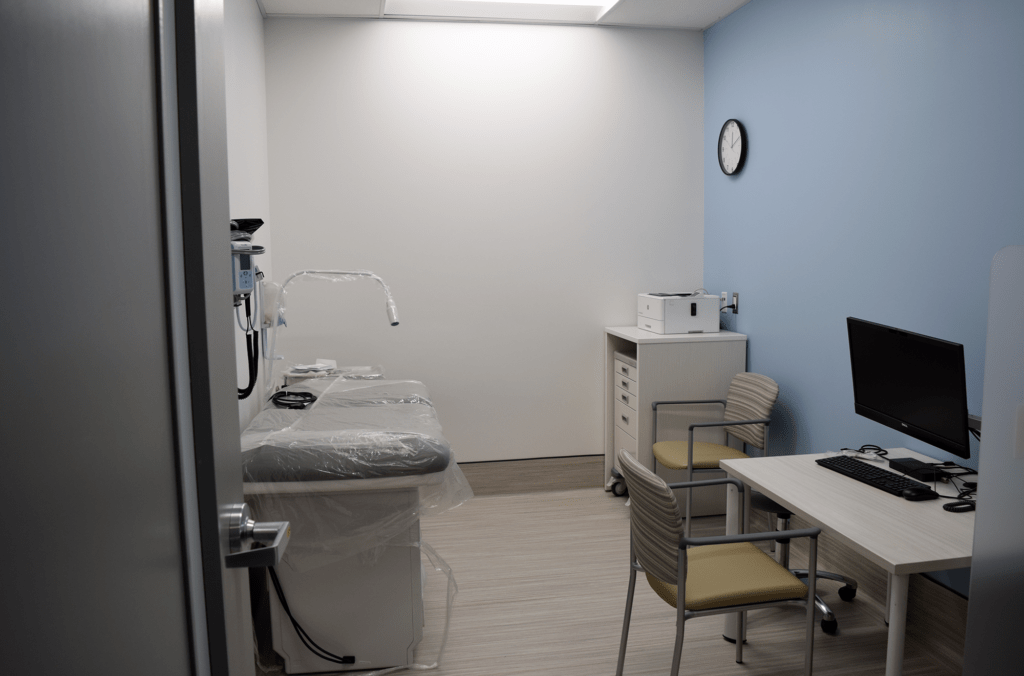
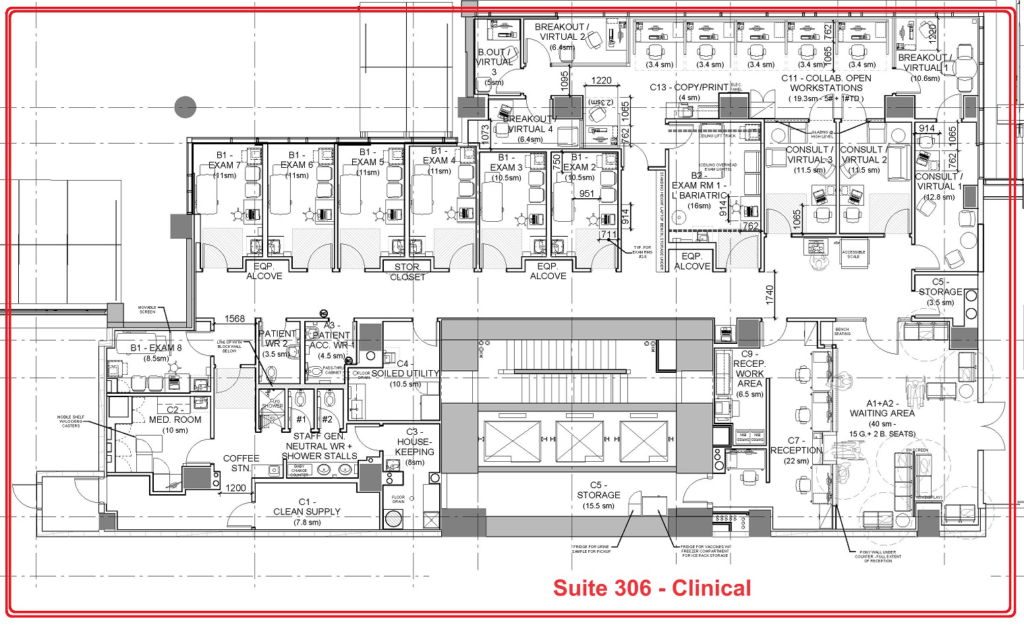
This new clinic will operate as a patient medical home, becoming one of three services within the Edmonds Centre for Healthy Communities (CfHC).
The PCN Steering Committee (PCN SC) will be awarding the contract to operate this clinic at the Edmonds CfHC to a Burnaby not-for-profit entity with expertise in delivering community-based social services to one or more of the populations, that will be served at the Burnaby Patient Medical Home for Priority Populations clinic (PPC).
The goal is to attach Burnaby residents from priority populations, as identified by PCN SC, to Primary Care Providers at the PPC. A core value of the Burnaby PCN is that addressing the social determinants of health is key to the development of healthy communities. As such, the clinic will target four priority populations: newcomers and refugees, expectant/new parents and their babies, residents with complex mental health needs, and homeless and/or underhoused residents.
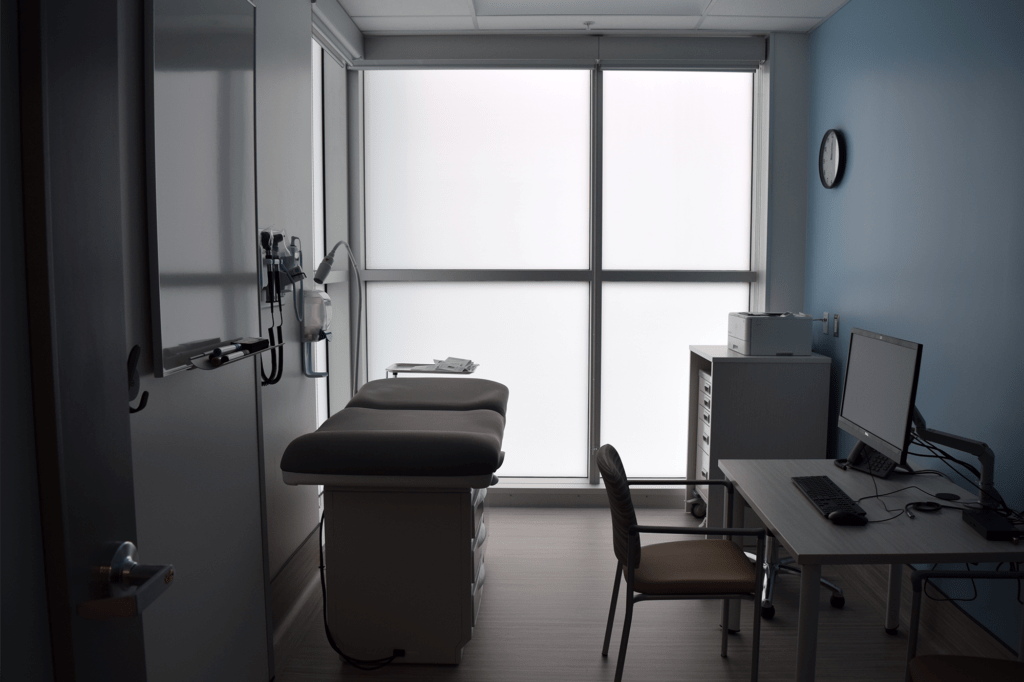
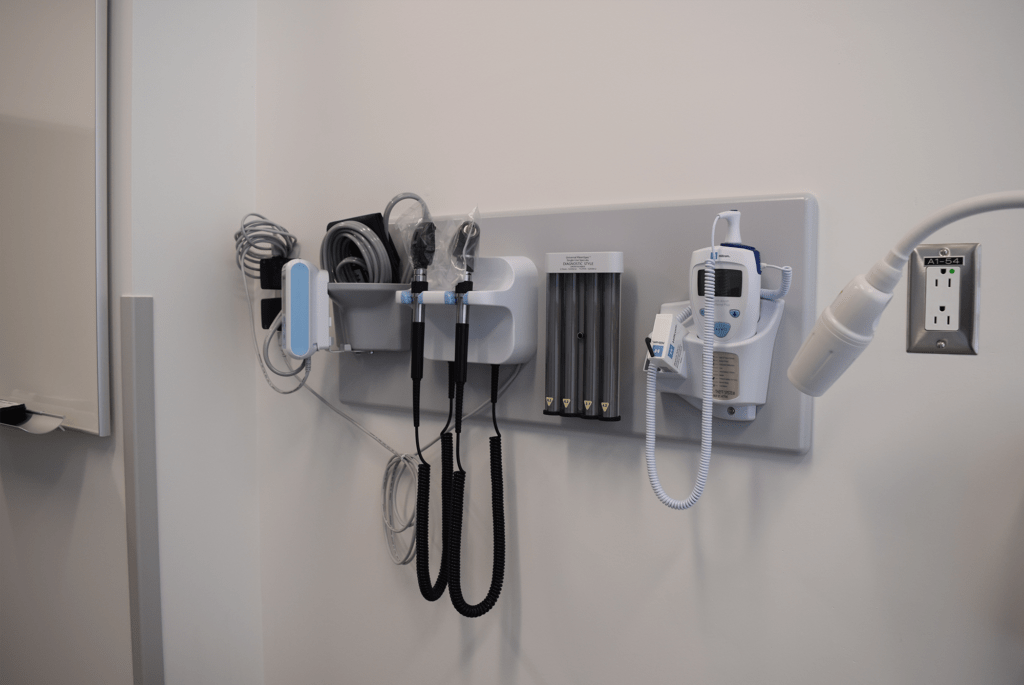
To support providing services to these populations, the clinic will operate in Primary Care Teams with on-site allied health and nursing staff working alongside family physicians (FPs) and Nurse Practitioners (NPs). The clinic will also be the home of a new maternity post-partum service that will be operated as an extension of the Burnaby Maternity Clinic (located at Burnaby Hospital).
A guiding principle of this funding opportunity is that the clinic will serve priority populations and that the clinic is an integral part of the network of family practice clinics and services in Burnaby. It will also deliver services to the surrounding family practices with patients within the identified priority populations. The successful not-for-profit is also expected to connect the services offered at the PPC to community-based services offered by the not-for-profit, and other social service organizations in the Burnaby community.
The successful not-for-profit would work alongside and govern the clinic in partnership with the family physicians, Fraser Health, and other local not-for-profits. This includes the initial setup and ongoing operations of the clinic.
Please read the Burnaby Patient Medical Home for Priority Populations RFQ Guidelines for complete eligibility details, terms and conditions prior to completing your submission.
Questions from interested not-for-profits can be directed to [email protected] during the open application process.
APPLICATION PERIOD
Application period opens, Response Template available: October 18, 2023 at 12:00pm
Submissions due by: November 29, 2023 at 11:59pm
TO SUBMIT
Please read the submission guidelines in their entirety prior to filling out the submission template (available starting October 18). Applications can be submitted via email to [email protected] during the application period specified above.
Information Sessions
| Information Session #1 (Zoom meeting) | October 18, 2023 at 1:00pm | completed |
| Information Session #2 (Zoom meeting) | October 26, 2023 at 4:00pm | completed |
| Information Session #3 – Site Walkthrough (in-person) | October 27, 2023 at 3:30pm | completed |
| Information Session #4 – Site Walkthrough (in-person) | November 16, 2023 at 4:00pm | completed |
| Community Providers Forum — open to input from all Burnaby community providers, including non-applicants | November 20, 2023 at 3:00pm (in-person), 3:30pm (Zoom) | completed |
FAQs
Any questions from the information sessions or questions submitted by email will be posted publicly on this webpage.
What is the difference between the priority populations clinic and a Community Health Centre?
Primary Care Providers working in Community Health Clinics generally have patient attachment targets that are reduced in order to best support priority populations. As the Burnaby PPC does not currently have CHC status there is not reduced patient panel sizes. CHCs also have ongoing funding for a Director level role within their funding envelope, the Burnaby PPC has one year funded for a Director level role. The CHC application would include the request for an ongoing funded position.
What is clinical liability and what is management liability?
Primary Care Providers and Allied Health Clinicians have their own clinical liability and malpractice coverage inclusive of patient care. The not-for-profit operating the Burnaby PPC would still need to obtain insurance for the clinic space inclusive of: General Liability, Business Property Insurance, and Business Interruption Insurance (optional).
Is the concept of the Patient Medical Home (PMH) at the Edmonds Centre for Healthy Communities pre-existing, or is it an entirely new concept?
The concept of a Patient Medical Home (PMH) is not new and has been used in the BC context since 2016. The PMH at the Edmonds Centre for Healthy Communities is a completely new clinic. It would be the responsibility of the not-for-profit to operate this new clinic.
Is it accurate to describe the medical clinic as a walk-in clinic that prioritizes serving the four priority populations?
No, this would not be accurate. The clinic’s primary focus is on providing longitudinal family practice care to the four priority populations. There may be an aspect of care that provides episodic (walk-in) care, but the model’s main concept is patient attachment to the clinic, emphasizing having a regular health care team or provider for ongoing primary care needs.
Where are the attachment referrals coming from?
Referrals originate from a central attachment waitlist for Burnaby (currently held by the Division, which will merge with the provincial Health Connect Registry) serving as the initial point for identifying individuals in need of services. Multiple agencies also assist in adding people to this attachment list, creating a comprehensive process to connect individuals with the clinic’s services.
Is this open to all Burnaby residents?
The clinic’s services will be open to Burnaby residents on the attachment waitlist if they fall into one of the four specified populations.
Is the training clinic open to internationally educated nurses who are enrolled in bridging programs at KPU (Kwantlen Polytechnic University) and TRU (Thompson Rivers University)?
The eligibility for internationally educated nurses enrolled in bridging programs would be determined based on the specific requirements of the clinic and the nursing education they require.
Is there a possibility of including health literacy education in this clinic, especially considering the one-on-one patient-doctor exam room setup?
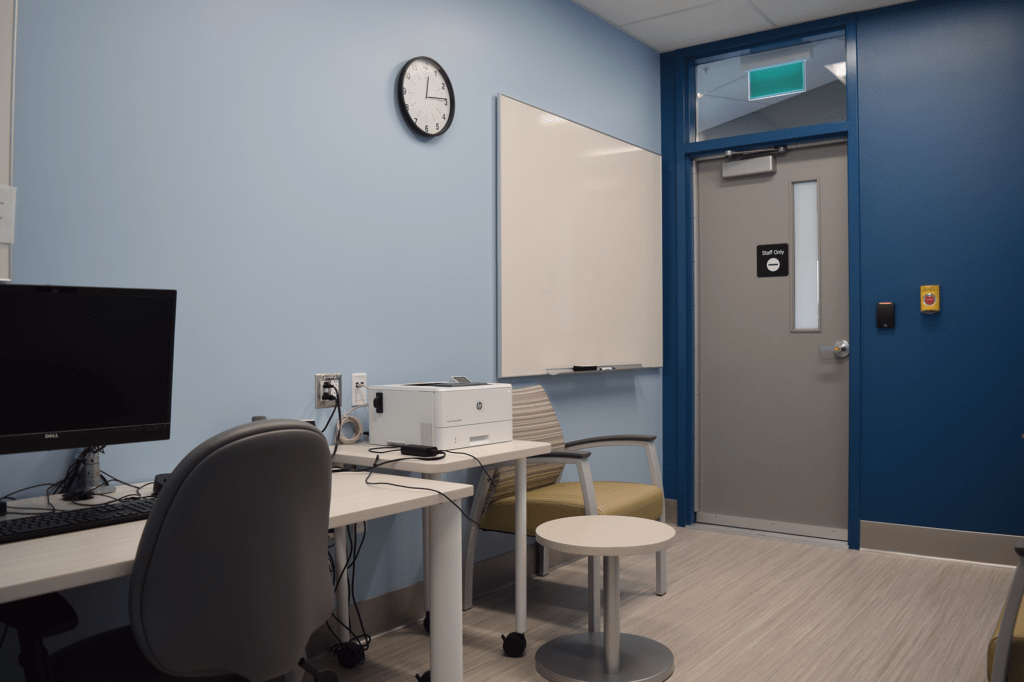
There is an open area within the clinic designated for group education sessions, which could potentially be used for health literacy education.
Will all the staff, including family physicians and nurse practitioners, be under the not-for-profit’s umbrella, or will they fall under the PCN (Primary Care Network)? Could you provide insight into the structure?
The HR manager, clinic director, allied health staff, and nursing staff will be employed by the not-for-profit operator(s) handling these hiring processes.
Family physicians and nurse practitioners will work as contractors. They will sign two agreements: one with Fraser Health for payment and another with the clinic (the not-for-profit) specifying their obligations, working hours, job scope, and the financial support they provide to the clinic’s operations.
The money to pay Nurse Practitioners (NPs) and Family Physicians (FPs) doesn’t flow through the clinic. Instead, the clinic receives a component of the money they earn, known as the overhead component. Their base pay, which is equivalent to a salary, is paid directly to them.
By what mechanism will primary care providers employed at the clinic be paid? And how will the clinic receive revenue?
The FPs are typically contracted for their hours and send invoices to Fraser Health for the hours they’ve worked. Fraser Health then pays them directly. The overhead component, which is revenue for the clinic, can be handled in two common ways, and the specific arrangement may vary and needs to be confirmed.
Will the steering committees (SC) consist of representatives from different organizations in Burnaby, including all these three committees? (CfHC Clinical SC, PPC Clinical SC and PCN SC)
PCC Clinical SC pertains to the PMH clinic.
The clinical steering committee will include representation from the entity (clinic) and family doctors within the network in Burnaby.
The entity is responsible for administrative management of the clinic, while doctors play a significant role in ensuring its clinical effectiveness. They work collaboratively to oversee the clinic and its integration with other components of the CfHC.
How does the Interim Federal Health Program (IFHP) fit into the committee’s structure? Will there be representation from IFHP on the committee, specifically for the IFHP-related aspects of the clinic’s operations?
The Interim Federal Health Program (IFHP) primarily relates to billing for government-sponsored refugees. While it’s possible for the clinic to register for IFHP for billing services for such refugees without MSP coverage, IFHP itself wouldn’t be part of the clinical steering committee.
How should we approach budgeting in the RFQ? Do we need to submit line budgets for each staff member, and if so, is there a reference or guidance document we can consult for this?
In the RFQ template, we didn’t specifically ask for a detailed budget for each staff member. We provided a cost breakdown based on equivalent salaries in the health sector. The revenue side of the budget is relatively fixed because it aligns with the funding structure from the ministry.
Will physician assistants be a part of this structure?
As of now, physician assistants are not available in primary care practice, but it may change in the future.
What will the operating hours be for this clinic?
The clinic’s operating hours have not been established yet. The decision on hours will be made collaboratively with the successful non-profit organization, considering the specific needs of the populations being served.
Is there an opportunity for the successful not-for-profit to establish satellite clinics?
If by “satellite clinics” you mean outreach services that use the PMH as home base, yes, the clinic will provide outreach services.
If by satellite clinics you mean additional medical clinic locations, this would require PCN SC approval and be dependent on funding availability and approval. These are not currently in scope.
Where do we draw the lines regarding electronic medical records (EMR) and what can be accessed by the not-for-profit in terms of privacy and confidentiality, considering this partnership between PCN and a not-for-profit organization?
You would follow the same rules as any other clinic. Only those who need to access a specific patient’s records should have access to them. Access to medical records should be limited to the individuals providing care for the patient in question.
Is there a component for ongoing evaluation within the project?
There will be an evaluation component (refer to RFQ guidelines document for discussion of the annual report). We could collaborate on a more frequent evaluation schedule if desired.
The reporting requirements for financial and HR aspects will be necessary due to the funding structure involving the Ministry of Health.
Will the Patient Medical Home, have a single management overseeing all three Edmonds CfHC sites under one umbrella, or will there be separate management teams working closely together?
The Edmonds CfHC consists of three key components:
- The Allied Health Hub, operated by Fraser Health and BDFP, is fully operational and will continue that way.
- The Patient Medical Home (PMH) for priority populations will be run by an NGO in partnership with Family Doctors, creating a medical clinic.
- There’s an Edmonds UPCC operated by family practice on behalf of the community
Is this funding coming as a global allocation, or is it part of the regular funding with specific allocations from the ministry? Can you clarify the nature of the funding in this context?
The funding is not a global allocation. The funding is broken down as follows:
- FP and NP positions
- Allied Health and Nursing positions
- Non-clinical staff positions
- Other operating costs
Revenue:
- The funding structure is not global; it involves targeted amounts for specific positions.
- Overhead or revenue includes a 15% addition to the salary of Allied Health positions.
- Estimated total overhead/revenue is approximately $645,000.
- Funding for Family Physician/Nurse Practitioner (FP/NP) contracts is not listed as it’s assumed that the health authority will directly fund these positions.
- Funding is provided for Allied Health and Nursing staff, and the clinic is responsible for their payroll.
- Direct funding from the Ministry of Health for targeted positions, such as Clinic Director, HR Manager, and Office Manager.
- PCN distribution funding is meant to address potential shortfalls in operating funds and is contingent on PCN overhead.
Expenses:
- The estimated cost of nursing and allied health staff is expected to match the funding for non-clinical staff, such as MOAs and support services.
- Lease costs are assumed to be covered by the health authority, with no cost passed on to the clinic.
- Other operating costs, such as equipment, supplies, EMR costs, internet, and phone costs, are estimated to be related to clinic operations.
- These expense estimates are based on real practice and represent typical clinic costs.
Could you provide additional details about the Edmonds UPCC?
The Edmonds Urgent Primary Care Centre (UPCC) is essential for the community, as it mainly specializes in offering urgent care services during evenings and weekends. Its services benefit both individuals who have primary care doctors and need after-hours care, as well as unattached patients seeking urgent medical attention. This facility plays a vital role in meeting the health care needs of the community, with a particular focus on unattached patients, and is a fundamental component of our health care services.
Is there an opportunity to explore a mixed staffing model, with the possibility of hiring nurses directly and having physicians employed through Fraser Health?
Nurse Practitioners (NPs) would follow the same contracting model as physicians. They would be contracted, and they would also sign a Practice Agreement.
The health authority is overseeing the contract, but they are not responsible for managing the connection or interaction between the family physician, the NP, and the clinic.
If the successful organization’s staff wages are already predetermined in our unionized environment, is it possible that they may not align with this funding model? If the numbers don’t match up as anticipated, how do we proceed with further discussions?”
The estimates in the funding table are based on salaries of equivalent positions in a unionized environment. Therefore, the salaries in your unionized setting should align reasonably well with these estimates, and significant discrepancies are not expected.
Is there a specific union that served as the basis for these estimates?
For nursing positions, the wage rates are determined based on the BCGU (British Columbia General Employees’ Union). The wage rates are generally standardized in line with ministry guidelines across different service offerings within the Primary Care Networks (PCN).